What Are Dermatomyositis and Polymyositis?
Dermatomyositis is an autoimmune disease where the body’s immune system attacks its own muscles and skin. Polymyositis is a closely related condition that affects only the muscles, without the skin involvement. Both are rare inflammatory myopathies - meaning they cause chronic inflammation in skeletal muscles, the ones you use to move your arms, legs, and neck. These aren’t just普通的 muscle soreness. The inflammation slowly weakens muscles over time, making everyday tasks like climbing stairs, lifting groceries, or even getting up from a chair become exhausting or impossible.
What makes dermatomyositis stand out is the rash. A distinctive purple or red rash often shows up on the eyelids - called a heliotrope rash - or over the knuckles, elbows, and knees. It’s not itchy or painful, but it’s unmistakable. Polymyositis doesn’t have this. If you see someone with unexplained muscle weakness and a rash like this, dermatomyositis is the first thing doctors look for.
These conditions don’t come out of nowhere. They’re autoimmune, meaning your immune system, which should protect you from germs, turns against your own body. In polymyositis, T-cells invade muscle fibers directly. In dermatomyositis, it’s more about antibodies and blood vessels - B-cells and inflammation around small blood vessels in the skin and muscle. This difference explains why treatments can vary and why one responds better to certain drugs than the other.
Who Gets These Conditions?
Polymyositis mostly hits adults between 30 and 60, with women being two to three times more likely to be affected than men. Dermatomyositis has a bimodal pattern: it can appear in children between 5 and 15, or adults in their 40s to 60s. There are no pediatric cases of polymyositis - if a child has muscle weakness and a rash, it’s almost always dermatomyositis.
It’s rare. About 1 to 7 people per 100,000 get polymyositis each year. Dermatomyositis is a bit more common, affecting 0.6 to 10 per 100,000. That’s why many general practitioners have never seen a case. This is a big reason why diagnosis takes so long - on average, people see four specialists and wait over two years before getting the right diagnosis. Many are initially told they have fibromyalgia, thyroid issues, or just "getting older."
One serious red flag: about 20% of adults diagnosed with dermatomyositis have an underlying cancer - often ovarian, lung, or colon cancer. That’s why, when dermatomyositis is diagnosed, doctors immediately order cancer screenings. Polymyositis doesn’t carry that same risk, so screening isn’t routine unless other symptoms suggest it.
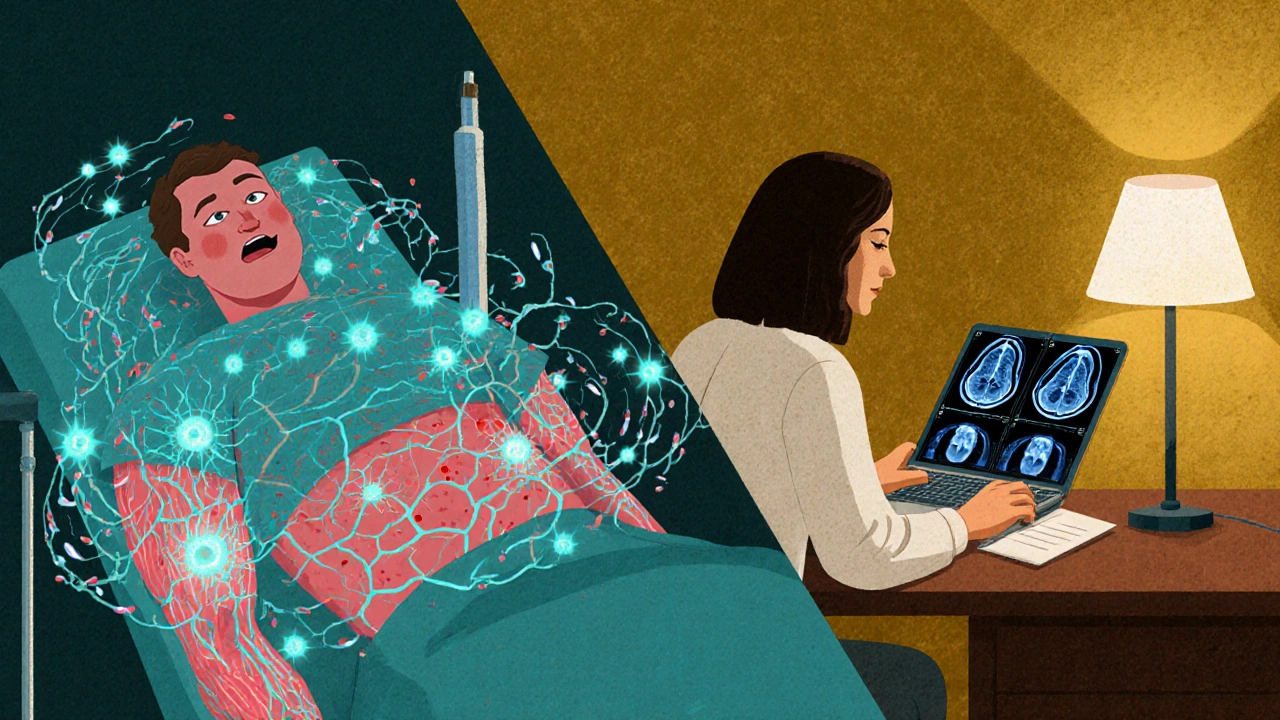
How Is It Diagnosed?
Diagnosis isn’t based on one test. It’s a puzzle. Doctors look at symptoms, blood work, imaging, and sometimes a muscle biopsy.
- Blood tests show high levels of creatine phosphokinase (CPK), often five to ten times above normal. Normal CPK is 10-120 U/L; in active disease, it can hit 8,000 or higher. Other markers like ESR and CRP show inflammation.
- Electromyography (EMG) measures electrical activity in muscles. In both conditions, it shows short, low-amplitude signals and spontaneous firing - signs of damaged muscle fibers.
- MRI can show swelling and inflammation in specific muscle groups, helping doctors decide where to biopsy.
- Muscle biopsy is the gold standard. In polymyositis, you see T-cells clustered around non-dead muscle fibers. In dermatomyositis, you see perifascicular atrophy - muscle fibers at the edges of bundles are wasting away - and inflammation around small blood vessels.
Since 2023, new classification criteria from EULAR now include myositis-specific antibodies (MSAs) as key diagnostic tools. These antibodies - like anti-Jo-1, anti-Mi-2, or anti-TIF1γ - aren’t just markers. They help predict disease behavior. For example, anti-TIF1γ is strongly linked to cancer-associated dermatomyositis. Testing for them cuts diagnostic delays by 30-40%.
What Does It Feel Like?
People don’t just feel weak - they feel trapped in their own bodies.
- Getting out of a chair? Hard. Climbing stairs? Impossible without holding on.
- Brushing hair or lifting a coffee cup? Arms feel like they’re filled with concrete.
- Swallowing becomes difficult - dysphagia affects 15-30% of patients. Food sticks, liquids go down the wrong way. This can lead to pneumonia if not managed.
- Fatigue is crushing. Not just tired - bone-deep exhaustion that doesn’t improve with rest. In one survey of over 1,200 patients, 68% said fatigue limited their daily life.
- For those with dermatomyositis, the rash can be socially isolating. People stare. Others assume it’s an allergy or infection. The emotional toll is real.
One Reddit user shared: "I used to run 5Ks. Now I can’t walk to the mailbox without stopping. I cry every morning because I know I’ll have to ask for help again today."
How Is It Treated?
There’s no cure. But with the right treatment, most people regain strength and live full lives.
First-line treatment: corticosteroids. Prednisone is the go-to. Doctors start with about 1 mg per kg of body weight - so 40-60 mg daily for most adults. This shuts down the immune attack quickly. Within 4-8 weeks, CPK levels should drop by half. Muscle strength often improves noticeably.
But steroids come with a heavy price. Long-term use leads to:
- Osteoporosis - 30-50% of patients lose bone density
- Diabetes - 15-30% develop insulin resistance
- Cataracts - 20-40% need eye surgery
- Weight gain, insomnia, mood swings
That’s why doctors don’t keep patients on high doses forever. They taper slowly - over months, sometimes years - while adding second-line drugs to reduce steroid dependence.
Second-Line and Advanced Therapies
If steroids alone aren’t enough - which they often aren’t - doctors add immunosuppressants:
- Methotrexate - the most common add-on. Slows disease progression and cuts steroid dose.
- Azathioprine - used when methotrexate causes liver issues.
- Mycophenolate mofetil - increasingly used for both conditions, especially if lung involvement is present.
- IVIG (intravenous immunoglobulin) - a blood product that resets immune activity. Works well in dermatomyositis, especially with severe skin disease or swallowing problems. Often used when other drugs fail.
- Rituximab - targets B-cells. Shown to help 60-70% of refractory cases in trials, though it’s still off-label for these conditions.
Recent breakthroughs include JAK inhibitors like tofacitinib. A 2023 trial showed 65% improvement in skin rash and 52% gain in muscle strength in dermatomyositis patients who hadn’t responded to anything else. Another drug, abatacept, is being tested for polymyositis and has shown promising early results.
The Role of Physical Therapy
Medication alone isn’t enough. Without movement, muscles waste away permanently.
Physical therapy starts within two weeks of diagnosis. It’s not about lifting heavy weights. It’s about gentle, consistent movement: seated leg lifts, resistance bands, walking. Studies show patients who stick with a tailored program improve functional capacity by 35-45% in six months. One man in Perth, diagnosed in 2024, went from needing help to stand to walking unassisted in 10 weeks - all because he did his daily exercises.
Therapists also teach breathing techniques and swallowing exercises for those with dysphagia. Speech pathologists are often part of the care team.

Living With It: Challenges and Realities
Even with treatment, life changes.
Side effects from meds are common. In one survey, 41% of patients had moderate to severe steroid side effects. Weight gain was reported by 82% of those affected. Insomnia hit 67%. Many stop taking their meds because they can’t handle the side effects - and then the disease flares again.
Insurance is another hurdle. Second-line drugs often require prior authorization. One study found delays averaged 17.3 days - time patients don’t have. In Australia, PBS subsidies help, but not all drugs are covered, and co-pays can be steep.
There’s also a shortage of rheumatologists. With only about 5,800 specialists for over 58 million Americans with autoimmune diseases, wait times are long. In Perth, patients often travel to Adelaide or Melbourne for specialist care.
What’s the Long-Term Outlook?
Twenty years ago, survival rates were under 60%. Today, they’re over 80% for dermatomyositis and 85% for polymyositis. Why? Earlier diagnosis. Better drugs. Aggressive treatment.
Experts agree: starting treatment within the first six months of symptoms gives you the best shot. One study found 80% of patients who got treated early reached low disease activity or remission. Delayed treatment? Higher risk of permanent muscle damage, lung scarring, or cancer complications.
Most people don’t go back to how they were before. But many regain enough function to work, drive, and care for their families. The key is consistency - taking meds, doing therapy, monitoring symptoms, and staying in touch with your care team.
What Should You Do If You Suspect It?
If you have:
- Progressive weakness in hips, shoulders, or neck - especially if it’s on both sides
- A purple or red rash on eyelids, knuckles, or knees
- Unexplained fatigue or trouble swallowing
Don’t wait. See your doctor. Ask for a CPK blood test. If it’s high, ask for a referral to a rheumatologist. Don’t settle for "it’s just aging" or "you’re stressed."
Early action saves muscles. And muscles? They’re your freedom.
Can dermatomyositis or polymyositis be cured?
No, there is no cure. But with early and aggressive treatment, most people achieve remission or low disease activity. Muscle strength can return, and many live full, active lives. The goal is control, not cure.
Is muscle weakness in these conditions always symmetrical?
Yes. Unlike other muscle diseases like inclusion body myositis, weakness in dermatomyositis and polymyositis is almost always symmetrical - affecting both sides of the body equally. This helps doctors rule out other conditions.
Why is a muscle biopsy necessary?
Blood tests and EMG can suggest myositis, but only a biopsy shows exactly what’s happening inside the muscle. It confirms inflammation type, rules out other diseases like cancer or infection, and helps distinguish between dermatomyositis and polymyositis - which guides treatment.
Can children get polymyositis?
No. Polymyositis only occurs in adults. Children with muscle weakness and a rash have dermatomyositis - sometimes called juvenile dermatomyositis. It’s a different disease with its own treatment protocols.
Do I need to avoid the sun if I have dermatomyositis?
Yes. Sunlight can trigger or worsen the rash. Even on cloudy days, UV exposure matters. Wear broad-spectrum sunscreen (SPF 50+), wide-brimmed hats, and UV-blocking clothing. Avoid direct sun between 10 a.m. and 4 p.m.
What happens if I stop my medication?
Stopping meds without medical supervision almost always leads to a flare. Muscle weakness returns, CPK levels spike, and recovery takes longer. Always taper under your doctor’s guidance - never quit cold turkey.
Are there new treatments on the horizon?
Yes. JAK inhibitors like tofacitinib are already showing strong results in trials for dermatomyositis. Abatacept and other targeted biologics are being tested for polymyositis. Researchers are also exploring gene therapies and stem cell transplants for severe, treatment-resistant cases - though these are still experimental.
Alex Czartoryski
November 19, 2025 AT 02:12
I've seen this disease take down three people I know. One was a gym coach who couldn't lift his own kid. Another, a teacher, had to quit because she couldn't hold a pen. The rash? Looks like a bruise that won't fade. No one believes you until you can't stand up. It's not just weakness-it's betrayal by your own body.
Victoria Malloy
November 20, 2025 AT 15:09
I was diagnosed last year. Started on prednisone and it felt like I was being slowly turned into a different person-weight gain, insomnia, mood swings. But PT saved me. Five minutes of leg lifts every morning. Now I can walk my dog without crying. It’s not a cure, but it’s a life.
Gizela Cardoso
November 21, 2025 AT 20:19
My mom had dermatomyositis. The hardest part wasn’t the weakness-it was the silence. People would say, 'You look fine!' like that meant anything. The rash made her feel like a freak. She stopped going out. I wish more doctors understood how much the emotional toll matches the physical.
Andrea Johnston
November 23, 2025 AT 05:59
Let me guess-you’re one of those people who thinks JAK inhibitors are magic. They’re not. They’re just another expensive band-aid. The real problem? Pharma is milking this. IVIG costs $20K a dose. Insurance denies it for months. Meanwhile, patients are dying because they can’t swallow their own meds. This isn’t medicine-it’s a profit pipeline.
Scott Macfadyen
November 23, 2025 AT 16:45
My cousin got diagnosed after her eyelids turned purple. Doc said 'maybe fibromyalgia' for a year. She finally got a biopsy in Toronto. Turned out her CPK was 9,200. Now she’s on rituximab and actually sleeping through the night. If you’re weak and rashy-don’t wait. Go to a rheum. Now.
Chloe Sevigny
November 25, 2025 AT 12:23
The pathophysiological divergence between T-cell-mediated myofiber invasion in polymyositis and humoral-driven perivascular inflammation in dermatomyositis is not merely academic-it dictates therapeutic stratification. The 2023 EULAR criteria, by codifying myositis-specific antibodies as diagnostic anchors, have fundamentally altered the prognostic landscape. Anti-TIF1γ, for instance, is not a biomarker but a sentinel for malignancy-a paradigm shift in clinical triage.
Denise Cauchon
November 25, 2025 AT 17:59
This is all a lie. The government is using this to push vaccines. Look at the timing-right after the pandemic. Why do they always target muscles? Because that’s where the implants are. You think your weakness is from autoimmunity? It’s from 5G and chemtrails. They’re testing on us. Don’t take their drugs. Eat turmeric and pray.
Erica Lundy
November 27, 2025 AT 11:45
The temporal correlation between disease onset and cancer diagnosis in dermatomyositis remains statistically significant, even after controlling for age and sex. While the causal mechanism remains incompletely elucidated, the presence of anti-TIF1γ antibodies constitutes a robust predictive marker. Early oncologic surveillance, therefore, is not merely prudent-it is ethically imperative.
Kevin Jones
November 27, 2025 AT 16:08
Biopsy is gold. No debate. EMG and CPK? Suggestive. But only tissue shows the perifascicular atrophy. That’s dermatomyositis. T-cells inside fibers? Polymyositis. Skip the biopsy? You’re guessing. And guessing kills muscles.
Premanka Goswami
November 28, 2025 AT 19:07
They don’t want you to know this. The real cause is glyphosate in your food. It’s in the bread, the beer, the tofu. It shuts down your mitochondria. The rash? Your body trying to expel the poison. The drugs? They’re just masking it. Go organic. Stop the chemicals. Then you’ll see real healing.
Alexis Paredes Gallego
November 29, 2025 AT 12:37
This whole post is Big Pharma propaganda. JAK inhibitors? They’re toxic. IVIG? Made from blood donors who were paid to lie about their health. The real cure? Fasting. Cold exposure. No meds. No doctors. Just primal living. They don’t tell you this because they make billions off your fear.